Understanding HAE
Not a real patient.
Genetic disease6
Inherited gene
Spontaneous
mutation
Types of HAE
There are two major subtypes of HAE, which present with the same signs and symptoms1:
85%
Type I
Characterized by low levels of antigenic
and functional C1 esterase inhibitor
15%
Type II
Characterized by normal antigenic and
low functional levels of C1 esterase inhibitor
HAE symptoms
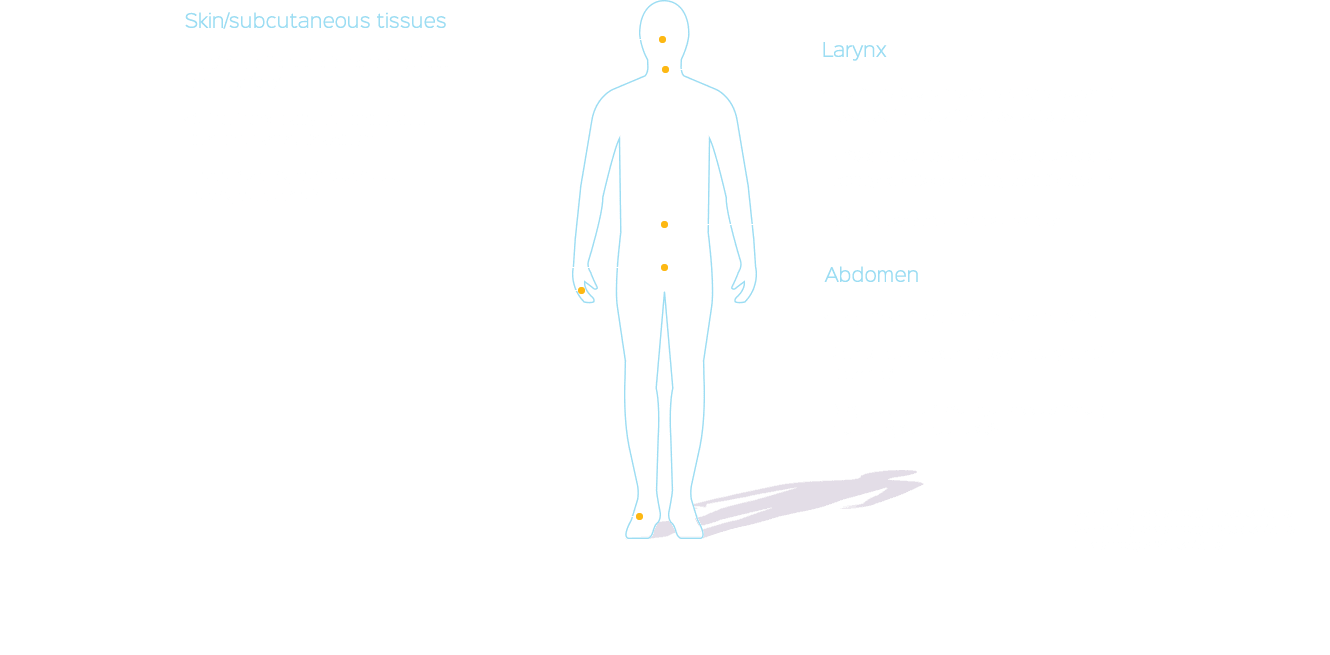
Attacks can be unpredictable, often occurring without a known trigger, and can migrate to other parts of the body during a single episode.1,4
The severity and frequency of HAE attacks vary greatly from patient to patient and can also change over time.1,2 Before an attack, some patients may experience a prodrome, often a tingling sensation in the affected area. HAE attacks usually present without urticaria or pruritus. When untreated, the swelling in an HAE attack typically increases over a 24-hour period and then gradually subsides during the next 48–72 hours.1
Triggers
Though each person will have a unique experience with HAE, some known triggers are:
- Stress4
- Physical trauma, surgery, or a dental procedure2,4
- Infection2,4
- Hormonal influences10
- Mechanical pressure8
HAE attacks can have consequences.
HAE attacks can be debilitating and, in the case of laryngeal attacks, potentially life threatening.4 On average, an untreated patient will experience 2 to 4 attacks per month,1 usually lasting 2 to 5 days each.3,11
- About 75% of patients experience an attack at least once a year§7
- In a survey from 2010, 19-24% of patients underwent unnecessary procedures as a result of misdiagnosis, including removal of appendix||12
- About 50% of HAE patients experience at least one laryngeal attack in their lifetime§7,8
Every patient with HAE, even those who have only experienced attacks in other locations, is still at risk for laryngeal attacks.1
§According to a survey of 209 patients
||In a survey of 313 patients
You might also be interested in:
References
- Zuraw BL. Clinical practice. Hereditary angioedema. N Engl J Med. 2008;359(10):1027–1036.
- Zuraw BL, Banerji A, Bernstein JA, et al. US Hereditary Angioedema Association Medical Advisory Board 2013 recommendations for the management of hereditary angioedema due to C1 inhibitor deficiency. J Allergy Clin Immunol Pract. 2013;1(5):458-467.
- Cicardi M, Bork K, Caballero T, et al. Evidence-based recommendations for the therapeutic management of angioedema owing to hereditary C1 inhibitor deficiency: consensus report of an International Working Group. Allergy. 2012;67(2):147-157.
- Banerji A. The burden of illness in patients with hereditary angioedema. Ann Allergy Asthma Immunol. 2013;111(5):329–336.
- Longhurst HJ, Bork K. Hereditary angioedema: causes, manifestations and treatment. Br J Hosp Med (Lond). 2006;67(12):654–657.
- Altman KA. Hereditary angioedema: a brief review of new developments. Curr Med Res Opin. 2014;30(5):923-930.
- Bork K, Meng G, Staubach P, Hardt J. Hereditary angioedema: new findings concerning symptoms, affected organs, and course. Am J Med. 2006;119(3):267-274.
- Agostoni A, Aygören-Pürsün E, Binkley KE, et al. Hereditary and acquired angioedema: problems and progress: proceedings of the third C1 esterase inhibitor deficiency workshop and beyond. J Allergy Clin Immunol. 2004;114(3 Suppl):S51–S131.
- Bork K, Staubach P, Eckardt AJ, Hardt J. Symptoms, course, and complications of abdominal attacks in hereditary angioedema due to C1 inhibitor deficiency. Am J Gastroenterol. 2006;101(3):619–627.
- Nielsen EW, Gran JT, Straume B, Mellbye OJ, Johansen HT, Mollnes TE. Hereditary angio-oedema: new clinical observations and autoimmune screening, complement and kallikrein-kinin analyses. J Intern Med. 1996;239(2):119-130.
- Lumry WR, Castaldo AJ, Vernon MK, Blaustein MB, Wilson DA, Horn PT. The humanistic burden of hereditary angioedema: Impact on health-related quality of life, productivity, and depression. Allergy Asthma Proc. 2010;31(5):407–414.
- Lunn ML, Santos CB, Craig TJ. Is there a need for clinical guidelines in the United States for the diagnosis of hereditary angioedema and the screening of family members of affected patients? Ann Allergy Asthma Immunol. 2010;104(3):211–214.
![CINRYZE® (C1 esterase inhibitor [human]) Logo](/dist/images/hdr-log3.png)
![CINRYZE® (C1 esterase inhibitor [human]) Logo](/dist/images/hdr-logo2.png)